Dear readers,
I have not been this angry and unsettled about a piece of pop culture since the Fear VR: 5150 Knotts Berry Farm debacle of September 2016. This afternoon, I happened upon a post made by one of my Facebook friends regarding a book series called “Dork Diaries,” which is aimed at children (particularly girls) aged 8 to 14. The protagonist is a 14-year-old girl named Nikki Maxwell and her life as a middle schooler.
Before I get into the meat-and-potatoes of this post, I want to warn you that the following images contain extremely discriminatory language that some readers may find upsetting. All images were provided via a good friend of mine on Facebook who is also a mental health advocate and fights like hell against the stigma. I respect her deeply and am grateful to her for bringing this to my attention.
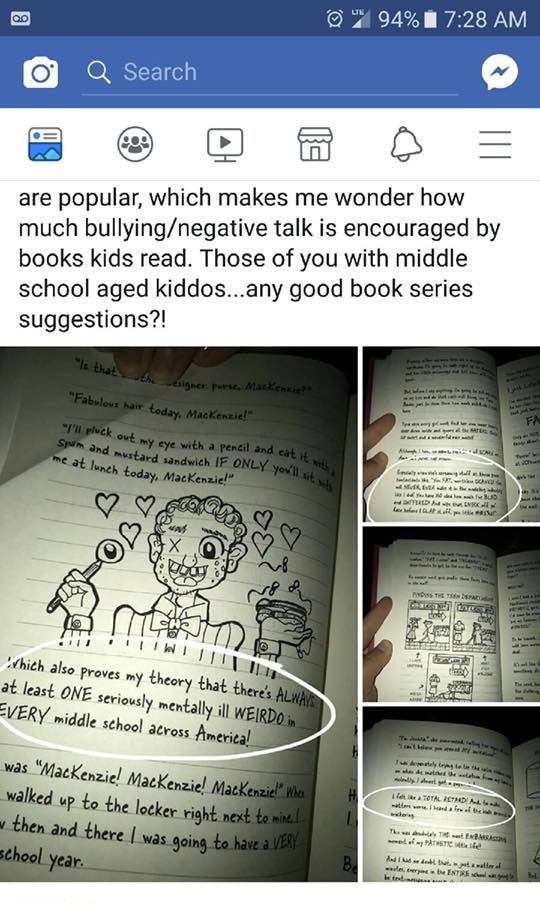
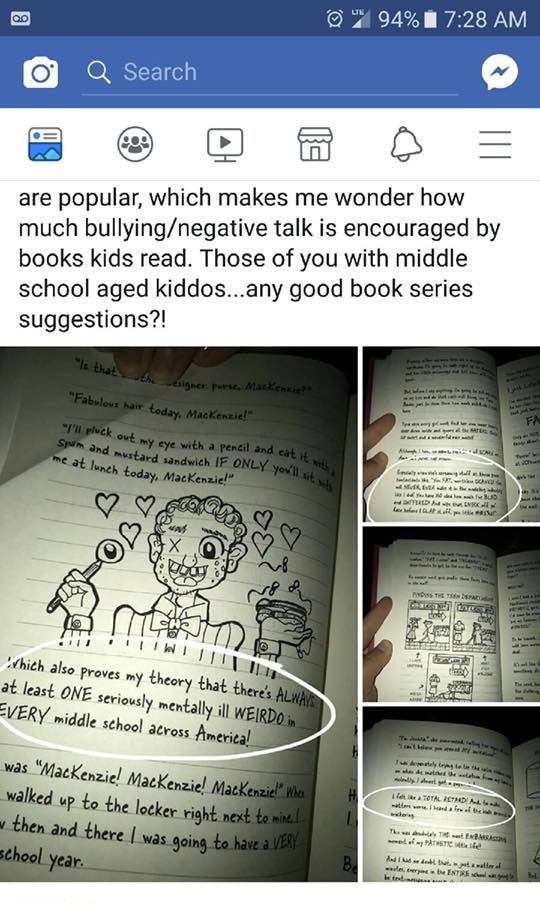
Below is the first image I saw regarding this series.
Let me begin by stating that I have not read any of the books in their entirety and had no idea they even existed until just a few hours ago. I also hate that by writing this post, I am giving this author more attention. However, I cannot let this issue go unaddressed for a number of reasons. For the sake of brevity, I’ve made a list:
- Stigmatizing language hurts all of us, and we need to knock it off. Seriously
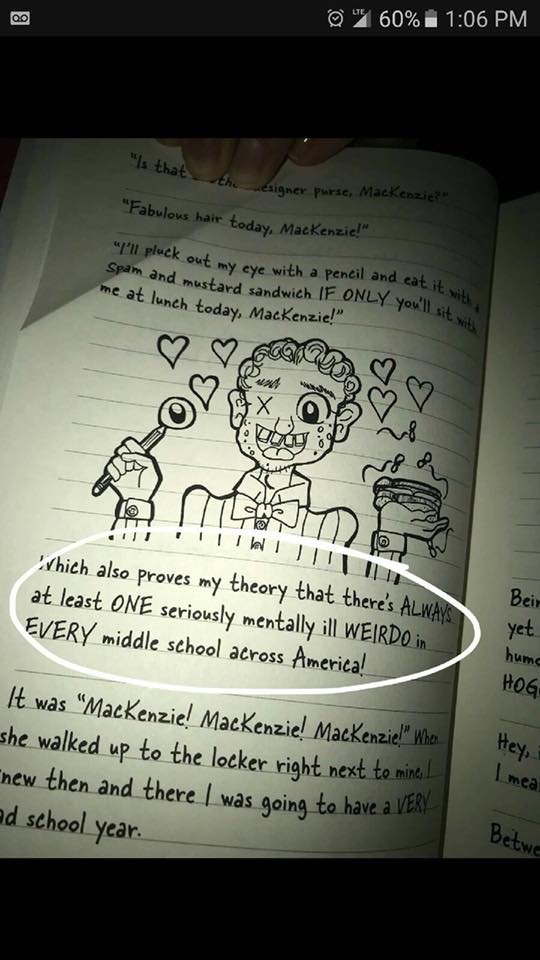
- The age range AND gender at which the books are targeted is highly disturbing, given the nature of the content. I’m not talking about the whole “celebrities being seen without panties but not phones” bit that many reviewers have cited as problematic.
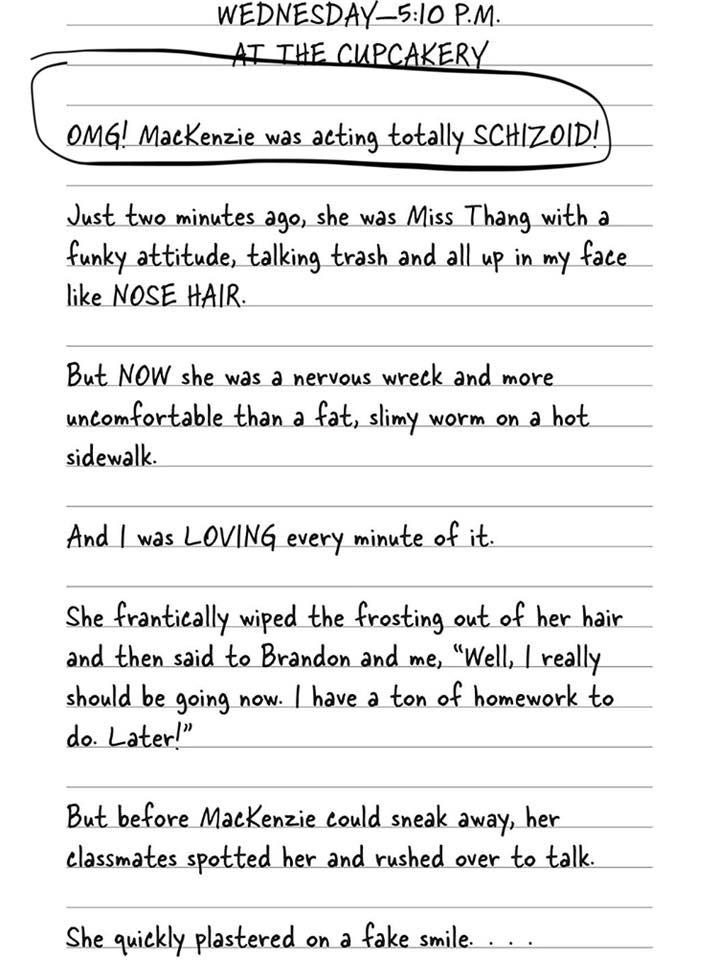
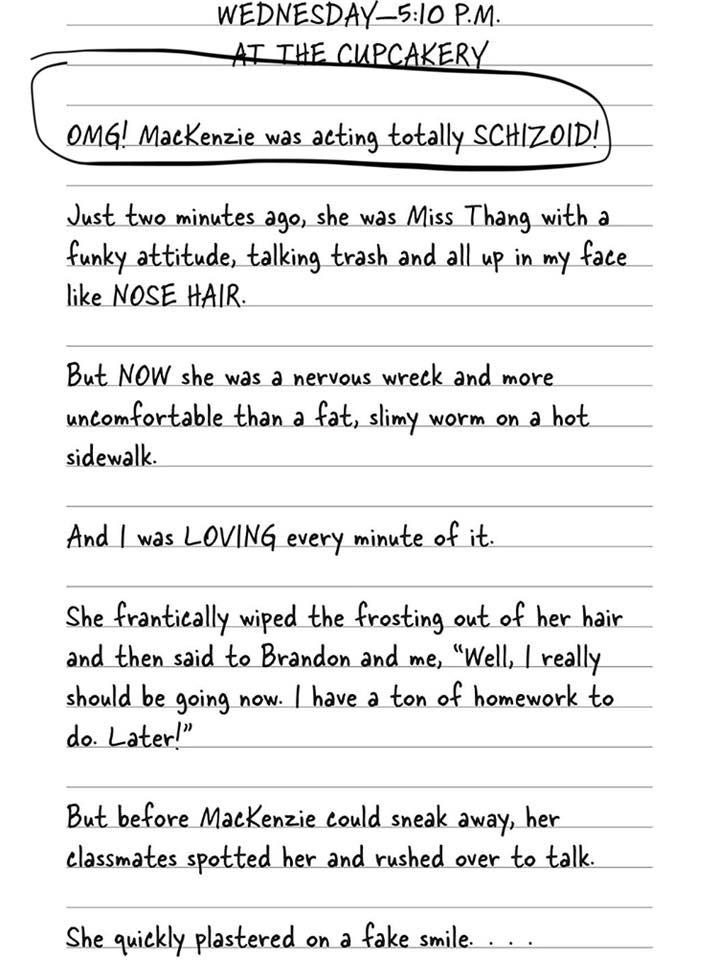
I’m talking specifically about the use of phrases such as “totally SCHIZOID!” etc. to describe the narrator’s peers. (I am also not 100% sure what the author means by “acting schizoid,” and I don’t think she does, either.)
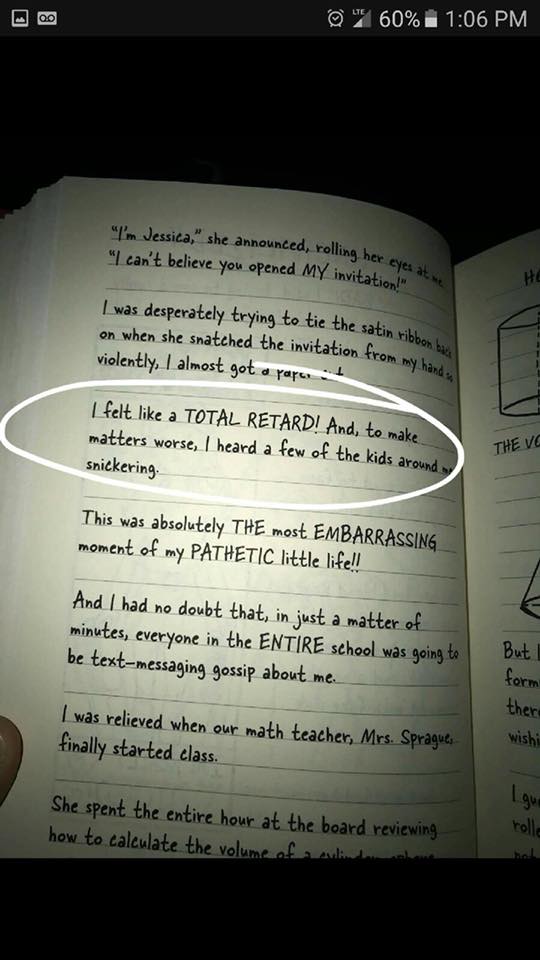
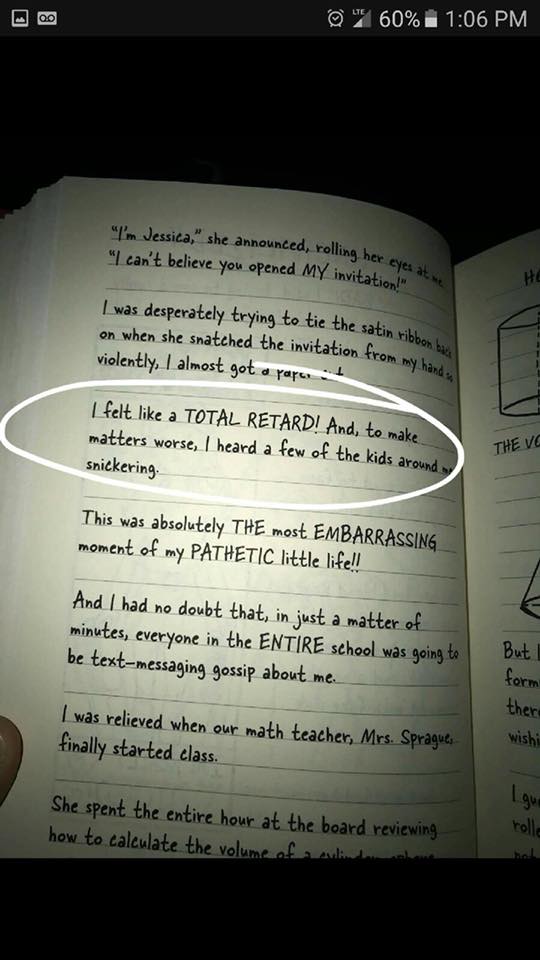
Dropping “RETARD” (please note the caps), even as a self-descriptor, is unacceptable. Come on, people. I thought we were better than this. The sad part is, the author could have gotten rid of the problematic language without negatively affecting the rest of the content. Cutting it would have actually made the book better. I’m wondering where the editor was in this process, if there even was one. I’m wondering why we still live in a world where this kind of thing manages to slip by largely uncontested.
- Where did the narrator (a 14-year-old girl) learn this language? Why does she think it’s okay to casually throw around such hateful, derogatory terms? Why isn’t this addressed in the book? And more importantly, why did the author think it was okay to write this in a children’s book without any sort of disclaimer?
Kids don’t come up with “you’re trash because X/Y/Z” on their own. They hear it from somewhere else, accompanied by the implication that it’s acceptable to dehumanize others for being different and perpetuate that toxicity ad infinitum. And this is a powerful reminder that none of us exist in a vacuum.
We can’t bubble-wrap our children, nor should we. There will always be bullies. There will always be stigma. But what we can do–what we must do–is educate ourselves and our children about the glorious range of people who share this planet with us. We must teach them accountability and respect. We must teach them that they are okay just the way they are and that the limitless expanse of diversity makes the world a far more beautiful, interesting, and magical place to live.
I am not in favor of censorship. What I am in favor of is self-awareness and recognizing when you’re about to fly off the rails and discriminate against an entire group of people in one broad stroke. Anyone who steps into the public eye has a duty to ensure that they are not causing harm to others. Context is also important. While this type of language would be a bit unsettling in a book written for adults (though I would take less issue with it given the audience and their assumed level of maturity and awareness), it is absolutely disturbing when it appears in a book written for children.
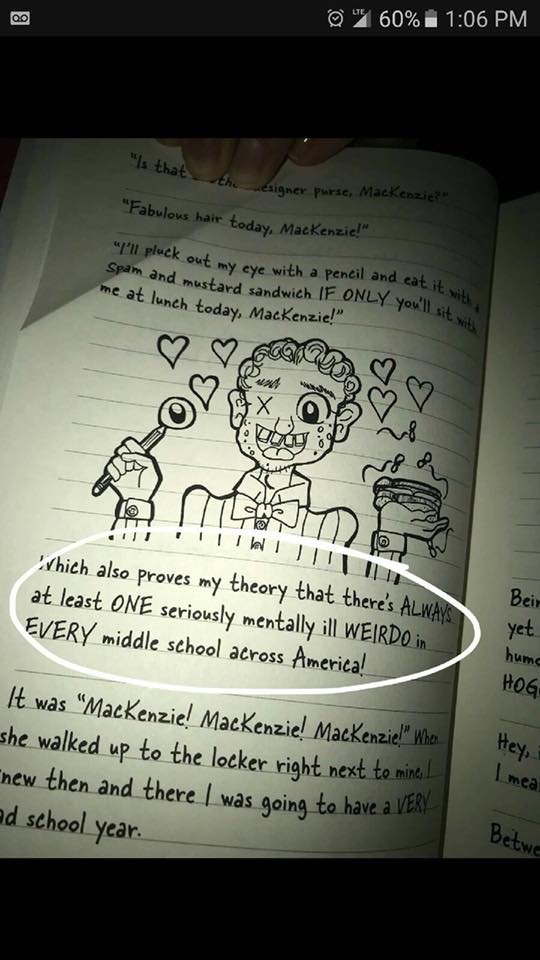
As a writer, an advocate, and a budding therapist, this sickens me. It’s lazy writing designed for shock value, to laugh at and “other” people who are living with mental illnesses and disabilities. Rachel Renée Russell’s writing is irresponsible at best, though I would go so far as to describe it as dangerous because these attitudes are dangerous. These attitudes have gotten people killed.
The one silver lining I can see is that a parent could pre-read the book, then use it as a jumping-off point for a discussion with their child (or children) about why such language is hurtful and not okay to use when describing another living, breathing, thinking, feeling human being.
Here’s an easy way to tell if you’re about to say something awful about another person. Take whatever adjective you were going to use–let’s say “schizoid,” for the sake of continuity–and replace that word with a group that has been historically discriminated against (but that society has collectively acknowledged was abused, stigmatized, and worse).
For example, the above passage would read “OMG! MacKenzie was acting totally JEWISH.” [Or “Black.” Or literally any other group that, when used as an adjective in a negative context, would make you look like a terrible person.]
That sounds bad, right? Does it make you feel really gross? It should. We may think we’ve conquered racism, sexism, anti-Semitism, all the other -isms…but we haven’t. We’ve barely even addressed them. All we’ve done is move on to another scapegoat, another bogeyman, another substitute that is slightly more socially acceptable but still conveys the level of disdain as older, more taboo slurs and epithets.
And what about the kids reading it who happen to have any of the conditions Russell has singled out in her books as targets of derision and malice? What happens when a child who has some form of mental illness or disability? How is a parent supposed to help heal the damage done when the hatred is right there in black and white for the child to see? The message sent by these books is that it’s acceptable to make people feel less-than because of something they cannot control.
And readers, you should never let anyone make you feel like less than you are, period. You are beautiful. Your brain is beautiful. You are strong. And we all deserve better than this.
With love,
One of those so-called mentally ill “weirdoes”
— J